
Catechol-O-Methyltransferase Inhibitors
General Information
Typically, the methylation of levodopa by catechol-O-methyltransferase (COMT) to 3-O-methyldopa is a minor pathway for levodopa metabolism. However, when peripheral dopamine decarboxylase is inhibited by carbidopa, a significant amount of 3-O-methyldopa is produced, which competes with levodopa for transport into the central nervous system (CNS). Entacapone and tolcaponeare the medicines that selectively and reversibly inhibit COMT. This inhibition leads to decreased plasma levels of 3-O-methyldopa, increased central uptake of levodopa, and higher brain dopamine levels. Both drugs reduce the “wearing-off” symptoms in patients on levodopa-carbidopa therapy. The primary differences between the two drugs are in their pharmacokinetics and adverse effect profiles.
Pharmacokinetics
Both entacapone and tolcapone are readily absorbed orally, unaffected by food, and are extensively bound to plasma albumin with limited distribution volumes. Tolcapone has a longer duration of action due to its affinity for the enzyme, while entacapone requires more frequent dosing. Both drugs are extensively metabolized and excreted in feces and urine. Dosage adjustments may be necessary for patients with moderate or severe cirrhosis.
Adverse Effects
Both drugs share adverse effects with levodopa-carbidopa, including diarrhea, postural hypotension, nausea, anorexia, dyskinesias, hallucinations, and sleep disorders. Tolcapone is associated with a serious risk of fulminant hepatic necrosis, thus it is reserved for patients who have not responded to other treatments, with regular liver function monitoring. Entacapone does not exhibit this toxicity and is commonly used in clinical practice.
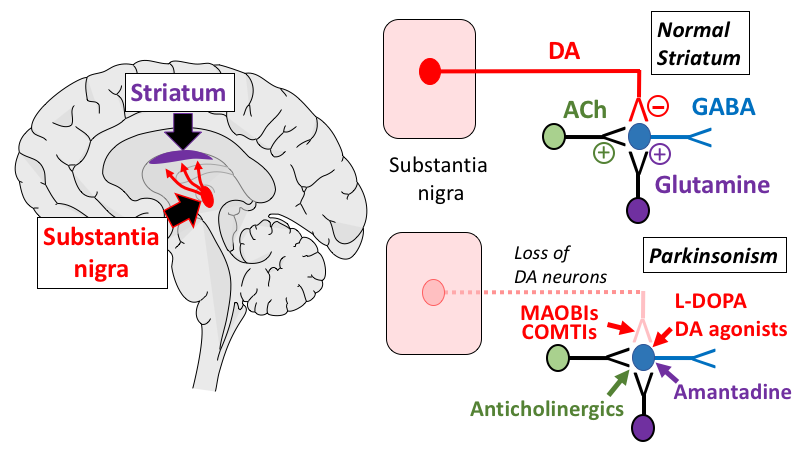
Dopamine Receptor Agonists
This group of anti-Parkinsonian drugs includes the ergot derivative bromocriptine and non-ergot drugs such as ropinirole, pramipexole, rotigotine, and apomorphine. These agents have a longer duration of action than levodopa, making them effective for patients experiencing fluctuations in response to levodopa. Initial therapy with these drugs carries a lower risk of developing dyskinesias and motor fluctuations compared to levodopa. Bromocriptine, pramipexole, and ropinirole are effective in managing motor fluctuations and dyskinesias in Parkinson’s patients. However, they are ineffective in patients unresponsive to levodopa. Apomorphine is used in severe and advanced stages to supplement oral medications. Adverse effects limit the use of dopamine agonists.
Bromocriptine
Bromocriptine, an ergot derivative, has actions similar to levodopa but more commonly causes hallucinations, confusion, delirium, nausea, and orthostatic hypotension, with dyskinesia being less prominent. It may worsen psychiatric conditions and should be used cautiously in patients with a history of myocardial infarction or peripheral vascular disease due to the risk of vasospasm. Bromocriptine can also cause pulmonary and retroperitoneal fibrosis.
Non-ergot Dopamine Agonists
Non-ergot dopamine agonists such as apomorphine, pramipexole, ropinirole, and rotigotine are approved for Parkinson’s treatment. Ropinirole is also indicated for restless legs syndrome. Pramipexole and ropinirole are orally active, while apomorphine and rotigotine are available as injectables and transdermal patches, respectively. Apomorphine is used for acute hypomobility “off” episodes in advanced Parkinson’s. Rotigotine provides even drug levels over 24 hours with a daily patch. These drugs are effective in both early and advanced Parkinson’s, delaying the need for levodopa and reducing its dose in advanced stages. They do not worsen peripheral vascular disorders or cause fibrosis. Adverse effects include nausea, hallucinations, insomnia, dizziness, constipation, and orthostatic hypotension, with less frequent dyskinesias compared to levodopa. Pramipexole requires dosage adjustments in renal dysfunction, and fluoroquinolone inhibitors of CYP450 1A2, like fluvoxamine, may necessitate ropinirole dose adjustments.
Amantadine
Amantadine, originally an antiviral drug, was found to have antiparkinsonian effects. It increases the release of dopamine, inhibits NMDA glutamate receptors, and has anticholinergic properties. Adverse effects include restlessness, agitation, confusion, hallucinations, and, at high doses, acute toxic psychosis. Other side effects are orthostatic hypotension, urinary retention, peripheral edema, and dry mouth. Amantadine is less effective than levodopa, with tolerance developing quickly, but it has fewer adverse effects.
Antimuscarinic Agents
Antimuscarinic agents like benztropine and trihexyphenidyl are less effective than levodopa and are used only as adjuncts in Parkinson’s therapy. These drugs block cholinergic transmission, helping to balance dopamine and acetylcholine activity. They can cause mood changes, confusion, dry mouth, constipation, and visual problems. These agents interfere with gastrointestinal motility and are contraindicated in patients with glaucoma, prostatic hyperplasia, or pyloric stenosis.
Conclusion
In the treatment of Parkinson’s disease, a variety of pharmacological strategies are employed to manage symptoms and improve patient quality of life. Catechol-O-methyltransferase (COMT) inhibitors, such as entacapone and tolcapone, play a crucial role in enhancing the efficacy of levodopa by preventing its peripheral methylation, thereby increasing central nervous system uptake and dopamine concentration. These inhibitors are particularly useful in reducing the “wearing-off” effects experienced by patients on levodopa-carbidopa therapy, although tolcapone’s use is limited due to its risk of severe hepatic toxicity.
Dopamine receptor agonists, including both ergot derivatives like bromocriptine and non-ergot drugs such as ropinirole, pramipexole, rotigotine, and apomorphine, offer alternative or adjunctive options to levodopa. These agents provide a longer duration of action, helping to manage motor fluctuations and reduce the incidence of dyskinesias associated with levodopa. Despite their benefits, their use is constrained by a range of adverse effects, including neuropsychiatric symptoms and orthostatic hypotension.
Amantadine, an antiviral drug with antiparkinsonian properties, provides modest benefits through multiple mechanisms, including increased dopamine release and NMDA receptor antagonism. However, its efficacy is limited compared to levodopa, and tolerance develops quickly.
Antimuscarinic agents, such as benztropine and trihexyphenidyl, serve as adjuncts to correct the imbalance between dopamine and acetylcholine in the brain. While they are less effective than levodopa, they can be useful in managing specific symptoms, though their use is limited by a range of anticholinergic side effects and contraindications in certain patients.
Overall, the selection of therapy for Parkinson’s disease is tailored to the individual patient’s needs, balancing efficacy and side effects, and often involves a combination of these pharmacological agents to optimize symptom control and improve functional outcomes.
