
Antihypertensive drugs act on one or more of four anatomical control sites to interfere with the normal regulation of blood pressure . These drugs can be classified based on their primary regulatory site or mechanism . Drugs in each category typically share similar toxicities due to their common mechanisms of action.
The categories are:
1. Diuretics: These reduce blood pressure by decreasing the body’s sodium levels, reducing blood volume, and possibly through other mechanisms.
2. Sympathoplegic Agents: These lower blood pressure by decreasing peripheral vascular resistance, inhibiting heart function, and increasing venous pooling in capacitance vessels, which reduces cardiac output. These agents are further divided based on their action sites in the sympathetic reflex arc.
3. Direct Vasodilators: These lower blood pressure by relaxing vascular smooth muscle, thereby dilating resistance vessels and, to varying extents, increasing capacitance.
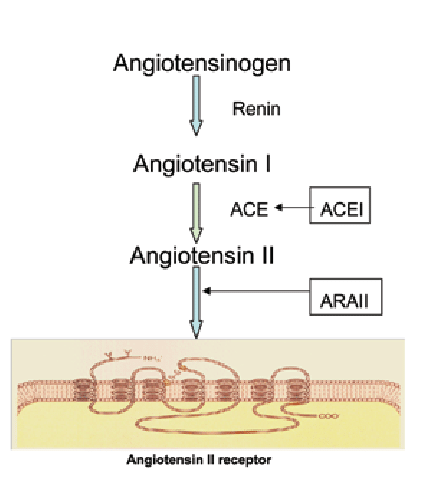
4. Agents Blocking Angiotensin Production or Action: These reduce peripheral vascular resistance and potentially decrease blood volume by inhibiting angiotensin.
Combining drugs from different categories is possible due to their distinct mechanisms of action.
Drugs That Alter Sodium and Water Balance
Dietary sodium restriction has long been known to reduce blood pressure in hypertensive patients. Although diuretics once made sodium restriction seem less crucial, it is now widely agreed that dietary control of blood pressure is a low-risk and potentially preventive measure. Even modest sodium restriction can significantly lower blood pressure in many hypertensive individuals.
Monotherapy vs. Polypharmacy in Hypertension
Monotherapy (using a single drug) for hypertension is preferable due to better compliance, lower costs, and sometimes fewer adverse effects. However, most hypertensive patients require multiple drugs acting by different mechanisms (polypharmacy). Up to 40% of patients may not respond adequately even to two drugs and may have “resistant hypertension,” necessitating three or more drugs. Some of these patients may have undiagnosed secondary hypertension, but most do not.
Rationale for Polypharmacy
- Compensatory Mechanisms: Many antihypertensive drugs trigger compensatory mechanisms that limit their effectiveness. For example, vasodilators like hydralazine significantly reduce peripheral resistance but cause compensatory tachycardia and salt and water retention, which can negate their effects. Combining a vasodilator with a beta-blocker can prevent tachycardia, and adding a diuretic can prevent salt and water retention, enhancing the overall efficacy.
- Maximum Efficacy: Some drugs have limited maximum efficacy. For instance, ACE inhibitors often reduce blood pressure by less than 10 mm Hg. Although this is insufficient for patients with stage 2 hypertension, ACE inhibitors have significant long-term benefits, such as reducing renal disease in diabetics and preventing heart failure.
- Toxicity at High Doses: The toxicity of some drugs at high doses prevents their use at these levels. The use of beta-blockers, for example, has been debated due to varying benefits among different drugs in the group. However, all beta-blockers help reduce mortality after a myocardial infarction, making them particularly useful for hypertensive patients with a history of infarction.
In practice, if one drug does not adequately control hypertension, a second drug from a different class with a different mechanism and toxicity profile is added. If necessary, a third drug can be added. If three drugs, typically including a diuretic, are insufficient, additional dietary sodium restriction and another drug may be required.
Conclusion on Antihypertensive Agents
Antihypertensive agents work by targeting various regulatory sites or mechanisms in the body to control blood pressure. These drugs can be classified into four main categories: diuretics, sympathoplegic agents, direct vasodilators, and agents that inhibit angiotensin production or action. Each category shares similar mechanisms of action and, consequently, similar toxicities.
Monotherapy, or the use of a single drug, is desirable for treating hypertension due to better patient compliance, lower costs, and potentially fewer side effects. However, many patients require multiple drugs from different classes (polypharmacy) to achieve adequate blood pressure control. This approach addresses the compensatory mechanisms that often diminish the effectiveness of single drugs.
In resistant hypertension, where two drugs are insufficient, a combination of three or more drugs, along with dietary sodium restriction, may be necessary. The rationale for using multiple drugs includes overcoming compensatory mechanisms, achieving maximum efficacy, and mitigating toxicity at higher doses.
Overall, the treatment of hypertension often involves a strategic combination of drugs to optimize efficacy and minimize side effects, with dietary modifications playing a supportive role.
