
Ganglionic Blockers
Ganglionic blockers target nicotinic receptors in both parasympathetic and sympathetic autonomic ganglia, and some also inhibit ion channels within these ganglia. These drugs do not distinguish between parasympathetic or sympathetic ganglia and are ineffective as neuromuscular antagonists. Consequently, they block all autonomic nervous system output at the nicotinic receptor. Apart from nicotine, the other drugs in this category are nondepolarizing, competitive antagonists. The effects of nondepolarizing blockers are varied and largely unpredictable, which limits their therapeutic use but makes them valuable in experimental pharmacology.
Nicotine
Nicotine, a toxic component of cigarette smoke, has no therapeutic use and is harmful to health. Depending on the dosage, nicotine first stimulates and then paralyzes all autonomic ganglia by depolarizing them. Its stimulatory effects are complex, involving increased neurotransmitter release due to its action on both sympathetic and parasympathetic ganglia.
Neuromuscular Blocking Agents
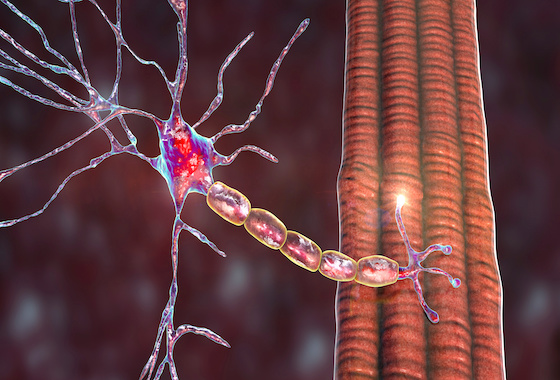
Neuromuscular blocking agents (NMBs) inhibit cholinergic transmission between motor nerve endings and nicotinic receptors on skeletal muscles. They share some chemical similarities with acetylcholine (Ach) and function as either antagonists (nondepolarizing) or agonists (depolarizing) at the receptors on the neuromuscular junction (NMJ). Clinically, NMBs are useful for rapid intubation in cases of respiratory failure, during surgery to facilitate endotracheal intubation, and for complete muscle relaxation at lower anesthetic doses, enhancing the safety of anesthesia. In the ICU, they are used to aid intubation and mechanical ventilation in critically ill patients.
Nondepolarizing (competitive) Blockers
The first known NMB was curare, historically used by Amazon hunters to paralyze prey. Tubocurarine was developed later but has been largely replaced by drugs with fewer side effects, such as cisatracurium, mivacurium, pancuronium, rocuronium, and vecuronium.
- Mechanism of Action:
- Low Doses: NMBs block Ach competitively at nicotinic receptors without stimulating them, preventing muscle cell membrane depolarization and inhibiting muscle contraction. This blockade can be overcome by cholinesterase inhibitors like neostigmine and edrophonium, which increase Ach concentration in the NMJ, shortening the duration of neuromuscular blockade. Muscle response to direct electrical stimulation from a peripheral nerve stimulator varies, allowing monitoring of neuromuscular blockade extent.
- High Doses: Nondepolarizing agents block motor end plate ion channels, further weakening neuromuscular transmission and reducing the effectiveness of cholinesterase inhibitors. With complete blockade, muscles do not respond to direct electrical stimulation.
- Actions: Muscles vary in their sensitivity to blockade by competitive agents. Small, fast contracting muscles of the face in addition to eye are most susceptible and paralyzed first, followed by the fingers, limbs, neck, and trunk muscles, then the intercostal muscles, and lastly, the diaphragm. Muscle recovery occurs in the reverse order. Sugammadex, a selective relaxant-binding agent, can speed recovery from rocuronium and vecuronium effects.
- Pharmacokinetics: All NMBs are administered intravenously or occasionally intramuscularly. Due to their bulky ring structure with multiple quaternary amines, they are poorly absorbed from the gut, do not penetrate membranes well, and do not cross the blood-brain barrier. Drug action is terminated in various ways. For instance, pancuronium is excreted unchanged in urine, cisatracurium undergoes organ-independent metabolism to laudanosine, which is further metabolized and excreted renally, and vecuronium and rocuronium are deacetylated in the liver and excreted unchanged in bile. Mivacurium is eliminated by plasma cholinesterase. The choice of agent depends on the desired onset, duration of muscle relaxation, and route of elimination.
- Adverse Effects: Generally, these agents are safe with minimal side effects, specific adverse effects are detailed in related documentation.
- Drug Interactions:
- Cholinesterase Inhibitors: Drugs like neostigmine, physostigmine, pyridostigmine, and edrophonium can counteract nondepolarizing NMBs’ actions, but increased Ach concentration may enhance depolarizing blockade. If the NMB is within the ion channel (bound to the receptor), cholinesterase inhibitors are less effective.
- Halogenated Hydrocarbon Anesthetics: Agents like desflurane enhance neuromuscular blockade by stabilizing the NMJ, sensitizing it to NMB effects.
- Aminoglycoside Antibiotics: Drugs like gentamicin and tobramycin inhibit Ach release by competing with calcium ions, synergizing with competitive blockers and enhancing neuromuscular blockade.
- Calcium Channel Blockers: These may increase the neuromuscular blockade of competitive blockers.
Depolarizing Agents
Depolarizing blocking agents, like succinylcholine, depolarize the muscle fiber’s plasma membrane similarly to Ach but resist degradation by acetylcholinesterase (AChE), resulting in persistent muscle fiber depolarization.
- Mechanism of Action: Succinylcholine binds to nicotinic receptors, acting like Ach to depolarize the junction. Unlike Ach, which is rapidly destroyed by AChE, succinylcholine remains at high concentrations in the synaptic cleft, causing sustained muscle cell depolarization. The duration of action depends on diffusion from the motor end plate and hydrolysis by plasma cholinesterase. Genetic variants with low or absent plasma cholinesterase levels can lead to prolonged neuromuscular paralysis. Initially, succinylcholine opens the sodium channel associated with nicotinic receptors, causing depolarization and transient muscle twitching (fasciculations). Continued binding leads to receptor inactivation, resulting in flaccid paralysis as the sodium channel closes or is blocked.
- Actions: Respiratory muscles are paralyzed last. Succinylcholine causes brief muscle fasciculations, leading to muscle soreness, which can be prevented by a small dose of nondepolarizing NMB prior to succinylcholine. Normally, succinylcholine’s action is short due to rapid hydrolysis by plasma cholinesterase. At the NMJ, it binds to nicotinic receptors, requiring redistribution to plasma for metabolism.
- Therapeutic Uses: Succinylcholine is used for rapid endotracheal intubation and during electroconvulsive shock treatment due to its rapid onset of action.
- Pharmacokinetics: Administered intravenously, succinylcholine’s brief action is due to rapid redistribution and hydrolysis by plasma cholinesterase, with effects disappearing quickly upon discontinuation.
- Adverse Effects:
- Hyperthermia: Succinylcholine can trigger malignant hyperthermia in susceptible patients.
- Apnea: In patients deficient in plasma cholinesterase or with an atypical enzyme form, succinylcholine can cause prolonged apnea due to diaphragm paralysis. Rapid potassium release may also contribute to prolonged apnea in patients with electrolyte imbalances. Caution is needed in patients with electrolyte imbalances receiving digoxin or diuretics.
- Hyperkalemia: Succinylcholine increases potassium release from intracellular stores, which can be dangerous for burn patients and those with massive tissue damage where potassium has been rapidly lost.**Conclusion:**
- Ganglionic blockers and neuromuscular blocking agents (NMBs) play distinct roles in pharmacology, affecting different aspects of the autonomic and somatic nervous systems. Ganglionic blockers, targeting nicotinic receptors in both parasympathetic and sympathetic ganglia, have limited therapeutic use due to their broad and unpredictable effects, though they are valuable in experimental settings. Nicotine, as a ganglionic blocker, exemplifies the potential for harmful effects without therapeutic benefits.
- In contrast, NMBs are clinically significant, especially in surgical and critical care settings. They facilitate procedures by blocking cholinergic transmission at the neuromuscular junction, leading to muscle relaxation. Nondepolarizing NMBs, such as curare derivatives, act as competitive antagonists, while depolarizing agents like succinylcholine mimic Ach but resist degradation, causing prolonged depolarization and muscle relaxation. Despite their utility, both classes of NMBs come with potential adverse effects and interactions with other drugs, necessitating careful management in clinical practice.
- Overall, while ganglionic blockers have limited clinical application, NMBs are indispensable in modern medicine for their ability to control muscle contraction during critical interventions, albeit with a need for careful monitoring and management of their side effects and interactions.
Conclusion:
Ganglionic blockers and neuromuscular blocking agents (NMBs) play distinct roles in pharmacology, affecting different aspects of the autonomic and somatic nervous systems. Ganglionic blockers, targeting nicotinic receptors in both parasympathetic and sympathetic ganglia, have limited therapeutic use due to their broad and unpredictable effects, though they are valuable in experimental settings. Nicotine, as a ganglionic blocker, exemplifies the potential for harmful effects without therapeutic benefits.
In contrast, NMBs are clinically significant, especially in surgical and critical care settings. They facilitate procedures by blocking cholinergic transmission at the neuromuscular junction, leading to muscle relaxation. Nondepolarizing NMBs, such as curare derivatives, act as competitive antagonists, while depolarizing agents like succinylcholine mimic Ach but resist degradation, causing prolonged depolarization and muscle relaxation. Despite their utility, both classes of NMBs come with potential adverse effects and interactions with other drugs, necessitating careful management in clinical practice.
Overall, while ganglionic blockers have limited clinical application, NMBs are indispensable in modern medicine for their ability to control muscle contraction during critical interventions, albeit with a need for careful monitoring and management of their side effects and interactions.
