
Hypertension, the most prevalent cardiovascular condition, was identified in 29% of American adults in a 2007/2008 survey. Its occurrence varies by age, race, education, and other factors. Studies indicate that 60-80% of both genders will develop hypertension by age 80. Chronic high blood pressure damages blood vessels in the kidneys, heart, and brain, leading to higher risks of renal failure, coronary disease, heart failure, stroke, and dementia. Effective blood pressure-lowering medications can prevent blood vessel damage, significantly reducing morbidity and mortality rates. However, surveys show that only 33-50% of Americans with hypertension have it under control. Numerous effective drugs are available, and understanding their mechanisms and action sites helps predict efficacy and side effects, allowing for safe and effective blood pressure management in most patients.
Diagnosis and Classification of Hypertension
Hypertension is diagnosed through repeated, reliable measurements of elevated blood pressure . This diagnosis mainly predicts future health issues rather than identifying the hypertension’s cause. Epidemiological studies show that the risk of damage to the kidneys, heart, and brain correlates with the level of blood pressure elevation. Even mild hypertension (blood pressure ≥140/90 mm Hg) increases the risk of organ damage. Starting from 115/75 mm Hg, the risk of cardiovascular disease doubles with each 20/10 mm Hg increase in blood pressure. Both systolic and diastolic hypertension can cause organ damage, and isolated systolic hypertension is also harmful. The urgency for treatment grows with higher blood pressure levels. The risk of organ damage is greater in African Americans and relatively lower in premenopausal women compared to men. Other risk factors include smoking, metabolic syndrome, obesity, dyslipidemia, diabetes, existing organ damage at diagnosis, and a family history of cardiovascular disease.
The diagnosis of hypertension is based on blood pressure measurements, not patient-reported symptoms. Hypertension is usually asymptomatic until significant organ damage is imminent or has occurred.
Causes of Hypertension
Specific causes of hypertension are identifiable in only 10-15% of cases. When no specific cause is found, it is termed essential or primary hypertension. When a specific cause is identified, it is called secondary hypertension. Identifying specific causes is important as some, like renal artery constriction, aortic coarctation, pheochromocytoma, Cushing’s disease, and primary aldosteronism, can be surgically treated.
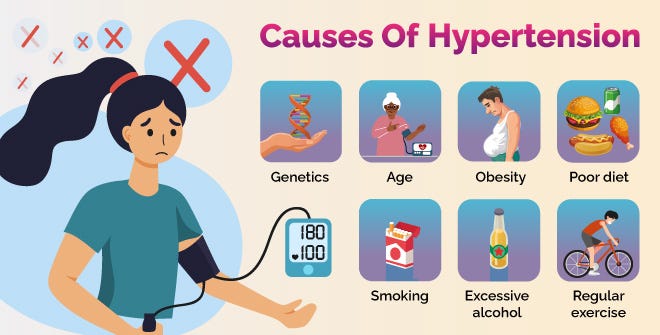
In most cases, high blood pressure is due to increased resistance in arterioles, while cardiac output remains normal. Studies of the autonomic nervous system, baroreceptor reflexes, the renin-angiotensin-aldosterone system, and the kidneys have not pinpointed a single cause for the increased peripheral resistance in essential hypertension. Instead, it appears to result from multiple abnormalities. Genetic factors, stress, and environmental and dietary factors (like high salt and low potassium or calcium intake) contribute to hypertension development. Populations with low sodium intake do not experience increased blood pressure with aging. Individuals with labile hypertension are more likely to have blood pressure spikes after salt intake.
The heritability of essential hypertension is estimated at 30%. Mutations in several genes are linked to rare hypertension causes, and variations in genes for angiotensinogen, ACE, the B₂ adrenoceptor, and α-adducin contribute to some essential hypertension cases.
Regulation of Blood Pressure
Arterial blood pressure (BP) is proportional to the product of blood flow (cardiac output, CO) and the resistance to blood flow through arterioles (peripheral vascular resistance, PVR):
BP = CO \times PVR
In both healthy and hypertensive individuals, blood pressure is regulated by adjusting cardiac output and peripheral vascular resistance. This regulation occurs at three anatomical sites: arterioles, postcapillary venules (capacitance vessels), and the heart. The kidneys also help maintain blood pressure by regulating blood volume. Baroreflexes, mediated by the autonomic nervous system, and humoral mechanisms, including the renin-angiotensin-aldosterone system, coordinate the function of these sites to maintain normal blood pressure. Additionally, local release of vasoactive substances from the vascular endothelium, such as endothelin-1 (which constricts blood vessels) and nitric oxide (which dilates them), may be involved in vascular resistance regulation.
In hypertensive patients, blood pressure regulation involves the same mechanisms as in normotensive individuals, but baroreceptors and renal blood volume-pressure control systems are set at a higher blood pressure level. All antihypertensive drugs work by interacting with these mechanisms.
Postural Baroreflex
Baroreflexes make rapid, moment-to-moment blood pressure adjustments, such as when moving from lying down to standing . Central sympathetic neurons in the medulla are continuously active. Carotid baroreceptors detect vessel wall stretch caused by arterial blood pressure, inhibiting central sympathetic activity. Reduced stretch, such as when standing up and blood pools in lower body veins, decreases baroreceptor activity, increasing sympathetic discharge. This reflex increases peripheral vascular resistance (arteriole constriction) and cardiac output (heart stimulation and capacitance vessel constriction), restoring blood pressure. This baroreflex also responds to events lowering arterial pressure, like vasodilator drugs or blood loss.
Renal Response to Decreased Blood Pressure
The kidneys control long-term blood pressure by regulating blood volume. Reduced renal perfusion pressure redistributes blood flow within the kidneys and increases salt and water reabsorption. Lower pressure in renal arterioles and sympathetic neural activity (via β adrenoceptors) stimulate renin production, increasing angiotensin II levels .Angiotensin II directly constricts resistance vessels and stimulates aldosterone synthesis in the adrenal cortex, increasing renal sodium absorption and blood volume. Vasopressin from the posterior pituitary gland also helps maintain blood pressure by regulating kidney water reabsorption.
Conclusion
Hypertension is a widespread cardiovascular condition affecting a significant portion of the American adult population, with prevalence influenced by age, race, and other factors. Chronic hypertension can lead to severe health issues, including renal failure, heart disease, and stroke, highlighting the critical need for effective blood pressure management. Despite the availability of numerous antihypertensive drugs and proven treatment strategies, many Americans fail to achieve adequate blood pressure control.
The diagnosis of hypertension relies on consistent measurements rather than symptoms, as the condition is typically asymptomatic until severe damage occurs. Both systolic and diastolic hypertension are harmful, and even mild elevations in blood pressure pose risks. Identifying the specific cause of hypertension is possible in a minority of cases, with most instances categorized as essential hypertension. The condition is usually multifactorial, with genetic, environmental, and dietary influences.
Blood pressure regulation involves complex mechanisms, including the role of the autonomic nervous system, renal function, and the release of vasoactive substances. In hypertensive individuals, these regulatory systems are often set at higher levels, necessitating medical intervention. The postural baroreflex and renal responses are key components of blood pressure control, adjusting rapidly to maintain stability and managing long-term blood volume.
