
Introduction
Alzheimer’s disease is characterized by three main features: the buildup of senile plaques (B-amyloid accumulations), the formation of numerous neurofibrillary tangles, and the loss of cortical neurons, especially cholinergic neurons. Current treatments aim to enhance cholinergic transmission in the central nervous system (CNS) or to prevent excitotoxic effects due to the overstimulation of NMDA-glutamate receptors in specific brain areas. Pharmacological interventions for Alzheimer’s disease target these mechanisms.
Alzheimer’s patients experience progressive cognitive decline due to the degeneration of brain cells. This degeneration leads to memory loss, confusion, difficulty with problem-solving, and changes in behavior and personality. As the disease advances, individuals may require assistance with daily tasks and eventually full-time care. Currently, there is no cure for Alzheimer’s disease, but treatments aim to manage symptoms and slow its progression. Care for Alzheimer’s patients often involves a combination of medication, therapy, and support from caregivers and healthcare professionals.
Acetylcholinesterase inhibitors
The progressive loss of cholinergic neurons is linked to the memory loss that is a hallmark of Alzheimer’s disease. It is believed that inhibiting acetylcholinesterase (AChE) within the CNS can improve cholinergic transmission in the remaining functional neurons. The reversible AChE inhibitors approved for Alzheimer’s treatment include donepezil, galantamine, and rivastigmine. These drugs show some selectivity for AChE in the CNS compared to the periphery. Additionally, galantamine may enhance acetylcholine’s action at nicotinic receptors in the CNS. These compounds may slow the rate of cognitive decline in Alzheimer’s patients modestly. Rivastigmine is the only AChE inhibitor approved for managing dementia associated with Parkinson’s disease and is also available as a transdermal patch. Unlike other AChE inhibitors, rivastigmine is broken down by AChE into a carbamylated metabolite and does not interact with drugs that affect CYP450 enzymes. Donepezil and galantamine are substrates for CYP450 and may interact with drugs affecting these enzymes. Common side effects of these inhibitors include nausea, diarrhea, vomiting, anorexia, tremors, bradycardia, and muscle cramps.
NMDA receptor antagonist
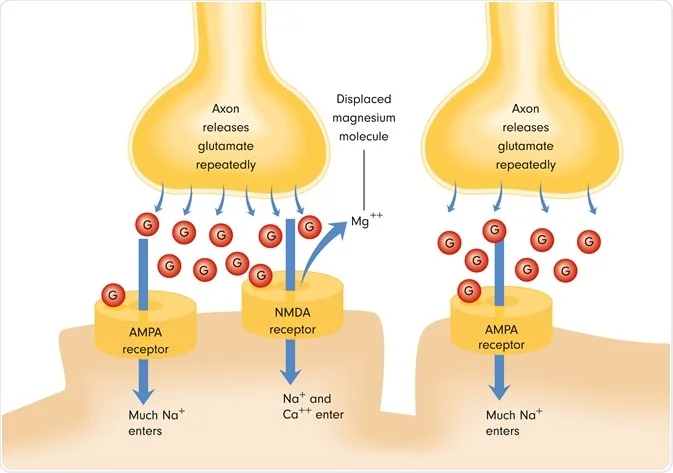
Glutamate receptor stimulation in the CNS is essential for forming certain memories. However, overstimulation, especially of NMDA-type receptors, can lead to excitotoxic effects on neurons, contributing to neurodegeneration or apoptotic processes. Glutamate binding to the NMDA receptor opens an ion channel, allowing Ca2+ to enter the neuron. Excessive intracellular Ca2+ can activate processes that damage neurons and cause apoptosis. ,NMDA Memantine receptor antagonist, is the drug utilize for moderate to severe Alzheimer’s disease. It blocks the NMDA receptor, reducing Ca2+ influx into the neuron to prevent toxic intracellular levels. Memantine is generally well-tolerated, with few dose-dependent side effects. Adverse effects such as confusion, agitation, and restlessness are often indistinguishable from Alzheimer’s symptoms. Due to its different mechanism of action and potential neuroprotective effects, memantine can be combined with an AChE inhibitor for treatment.
Conclusion
The pharmacological treatment of Alzheimer’s disease primarily targets two pathways: enhancing cholinergic transmission and preventing excitotoxicity due to NMDA receptor overstimulation.
- Cholinergic Enhancement: AChE inhibitors, such as donepezil, galantamine, and rivastigmine, are used to improve cholinergic transmission by inhibiting the breakdown of acetylcholine. These drugs can modestly slow cognitive decline, though they come with side effects like nausea and muscle cramps. Rivastigmine is unique in being used for Parkinson’s-related dementia and available in a transdermal form.
- Excitotoxicity Prevention: Memantine, an NMDA receptor antagonist, helps protect neurons by preventing excessive calcium influx, which can cause cell damage and apoptosis. Memantine is suitable for moderate to severe Alzheimer’s disease and has a favorable side effect profile, making it a good candidate for combination therapy with AChE inhibitors.
Overall, these treatments offer a modest benefit in slowing the progression of Alzheimer’s symptoms, highlighting the ongoing need for more effective therapies.
Commonly asked questions
1. What are the three main features characterizing Alzheimer’s disease?
– Accumulation of senile plaques (B-amyloid accumulations), formation of numerous neurofibrillary tangles, and loss of cortical neurons, especially cholinergic neurons.
2. Which pharmacological interventions aim to improve cholinergic transmission in the CNS for Alzheimer’s disease treatment?
– AChE inhibitors such as donepezil, galantamine, and rivastigmine.
3. What is the unique aspect of rivastigmine among AChE inhibitors in Alzheimer’s disease treatment?
– Rivastigmine is the only AChE inhibitor approved for managing dementia associated with Parkinson’s disease and is available as a transdermal patch.
4. How does memantine contribute to the treatment of Alzheimer’s disease?
– Memantine acts as an NMDA receptor antagonist, preventing excessive calcium influx into neurons and thus protecting against excitotoxicity.
5. What are some common side effects associated with AChE inhibitors in Alzheimer’s disease treatment?
– Nausea, diarrhea, vomiting, anorexia, tremors, bradycardia, and muscle cramps.
